Why You Should Get Evaluated for Obstructive Sleep Apnea
Treatment for OSA can change your life for the better.
I started snoring in my mid-thirties. It was a generational curse; my mother snored and had a CPAP (which she didn’t use), and my grandmother snored SO LOUDLY that my grandfather slept in a separate bedroom.
I’ve been trying for years to resolve my snoring. Over the past twelve years, I’ve had three sleep studies; in the first two, I didn’t qualify for treatment because I didn’t stop breathing enough times during the night. The threshold is > five times per hour; I was at 4.7.
Until this last sleep study, I’d looked for surgical ways to stop snoring, from removing that little dangling thing in the back of my throat to chemically stiffening the tissue of my soft palate, along with some other crazy, medieval-sounding torture. I couldn’t justify having that treatment because it wasn’t guaranteed to work.
Instead, I chose to wear a mouthguard. For many years, I went through all kinds of devices. At first, I got expensive ones through my dentist. I’d bite through them. I couldn’t keep paying for custom guards, so I started buying ones off Amazon for around $65. They worked fairly well for a while, even though I’d pull my mouthguard out of my mouth in the middle of the night and throw it across the bed. Too often, I’d be hunting in the covers for that contraption.
For the past few years, I’ve been tired. I’d wake up groggy and achy, and my head would be pounding. I’d take naps in the middle of the day. I could barely get through work, and I’d crash in bed when I got home.
Indeed, my lipedema was part of my symptoms, and after my surgery, I felt so much better. But, I continued to have problems sleeping, and in the morning felt like I’d woken from the dead.
Earlier this year, I decided to try another sleep study. I figured, “Why not? What did I have to lose?” I wasn’t confident this would go anywhere but made an appointment.
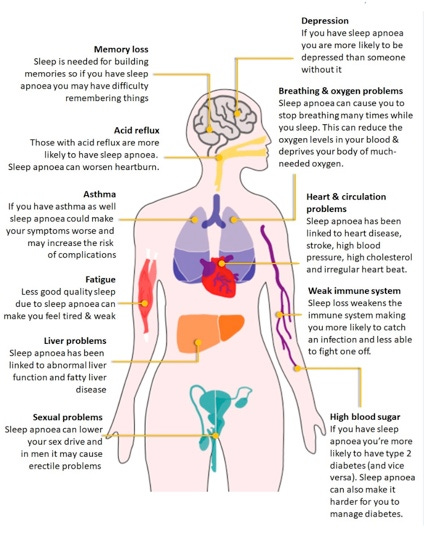
CPAP machines can help reduce the risk of several medical problems, including stroke and heart attack, high blood pressure, cardiovascular disease, and dementia.
A little side note: I started the process for my CPAP in March of this year. It took a couple of months to get the consult, another couple of months to get my actual sleep study, and then I had to wait a month for the results. Finally, it took another six weeks to actually get my machine. In total, it took me over five months. Five Months! Gotta love the U.S. healthcare system.
Anyway, my study results showed I stopped breathing, on average, 18 times per hour. When I was in REM sleep, that number increased to 42 times per hour. My longest apneic episode (where I stopped breathing) was 80 seconds. My oxygen saturation (normal is in the high 90s) went down to 78%. I have been diagnosed with moderate sleep apnea.
After twelve years and three sleep studies, I finally qualified for a CPAP. The third time’s a charm.
A couple of days ago, I passed my two-week mark of using my CPAP. Now I get up without grogginess or pain. I’m not tired all day. I was running, running, up the steps at work yesterday. I haven’t needed my daytime naps. I feel sharp. I feel like my usual self again.
Along with the complications listed in the above photo, untreated OSA is associated with lymphedema:
OSA and lymphedema
One study found that 74% of patients with lymphedema had OSA, and that the prevalence was higher for patients with lower limb lymphedema (85%) than upper limb lymphedema (56%).
OSA and chronic lymphedema
A literature review found that OSA is associated with chronic lymphedema.
OSA and leg edema
OSA is a probable cause of chronic leg edema, and treating OSA can reduce or eliminate swelling in patients with leg edema.
Source: JSV-VL
Also, if you start wearing CPAP, you can possibly reverse or partially reverse some complications of OSA.
Brain damage
CPAP therapy can reverse or partially reverse brain damage caused by OSA. Research shows that 12 months of CPAP therapy can almost completely reverse white matter damage. [1]
Appearance
Sleep apnea can cause you to look older due to stress hormones and lack of sleep. Treatment can reverse these effects, making you look more alert and younger. [2]
Daytime and nocturnal symptoms
CPAP can reverse daytime symptoms like sleepiness and nocturnal symptoms. [3]
Cardiovascular outcomes
CPAP therapy can reduce the risk of fatal and non-fatal cardiovascular outcomes in OSA. [4]

I will have to wear my CPAP for the rest of my life; CPAP is a treatment, not a cure.
Am I upset about hooking up a hose to my face every night? No, not for all of the benefits I’m now getting.
I was worried, though. I didn’t like the rumors I’d heard about CPAPs, only to find most of them were untrue.
I had a few misconceptions about my CPAP, ones that most people have:
Too Noisy: My CPAP has no noise. I mean, it is completely quiet. All you can hear is my breathing. I thought I would have to deal with an ongoing buzz, but nope. Even my husband says he has to check on me because he hears nothing over on my side of the bed. Although CPAPs are historically known to be noisy, they have improved the technology, and there is no machine noise whatsoever.
Too Uncomfortable: Yes, I have to strap the thing on my head. I have a mask over my face, but it’s a soft “pillow” plastic. Otherwise, it’s very comfortable.
The air pressure makes it hard to fall asleep: The CPAP has a gradient pressure that starts low and increases after I go to sleep. When I first put it on, the gentle air is mild, making it easier to fall asleep.
It takes a long time to get used to wearing a CPAP: I hear people quit using CPAPs because they can’t get used to them. My CPAP comes with an app that measures my usage. It helps me adjust my machine if I feel uncomfortable. I also have support from the technician who set up my machine. I can ask for unlimited help tweaking my machine to work for me. The technology now is incredible. It took me two nights to get used to my CPAP.
If you’ve been evaluated and found needing a CPAP, but it may have been a while ago, and you hated it because of any of the above reasons, please get re-evaluated. It will change your life.
I’m discussing surgery coverage at the Lipedema Simplified event on September 27-29th. I’ll be presenting on the 29th, along with Dr. Frank Labschies and other professionals in the lipedema community. Here’s the link to join:
Take care,
Michelle









When I went to Cleveland clinic, the physician suggested Sleep studies for all Lipedema patients. so I did. I was sort of borderline but I did get set up. Been on it 5 months. still adjusting but not hard. It hasn't made me feel any different but CPap changed my husband life. he even admits it to other men, like at golf etc. he couldn't stay awake anytime he sat down. he has more energy than any 70 yr old male I know.