You Don't Need to Pay Someone Hundreds of Dollars to Submit an Out-of-Network Request for Surgery
I'm spilling the tea! Other insurance experts don’t want you to know how easy this is, and I will save you hundreds of dollars!

We don't talk much about a part of the preauthorization submission that involves asking for your surgeon to be considered in-network so they can get paid for your surgeries. But this is as important as the preauth request.
Ironically, other lipedema “advocates” make thousands of dollars every year providing services for out-of-network exception submissions, off of Lipedema women who don’t know the insurance process.
When I learned that women were being charged hundreds of dollars solely for this particular task, I was appalled.
There is no need to pay another company hundreds of dollars to help with this part of your submission. You can do this yourself!
In fact, if you have been working to submit your preauth for liposuction surgery, the out-of-network (OON) request is a piece of cake.
And I will give you ALL the information you need for your OON request. Without paying other agencies hundreds of dollars for such a simple task.
How simple is it? Well, I’ll tell you…But first, let’s start at the beginning:
Being in-network means that the surgeon has an agreement with the insurance company to accept certain negotiated rates for services provided to patients covered by that insurance plan.
When you need to have your treating physician paid by your insurance and they do not already have a financial contract in place with them, they are considered out-of-network. That doesn’t mean you can’t go to the surgeon, but you must have a pretty good reason why you want to use that doctor over one your insurance is already contracted with.
In our case, most plastic surgeons don’t work with insurance and don’t have prearranged financial contracts with insurance. Most of their services are cosmetic and paid for out-of-pocket by their patients. However, with our surgeries, they aren’t cosmetic and should be covered by insurance. So, you and your surgeon must take that extra step to request insurance to consider the surgeon in-network.
Insurance will only consider this if no alternative surgeon in their network can perform the same surgery. And besides university hospitals that may have some contracted affiliations with insurances, they likely won’t have a plastic surgeon in network.
Requesting a network gap exception from your health insurer formally asks the insurer to cover care you get from an out-of-network provider at the in-network rate. The insurer considers these requests on a case-by-case basis. If your insurer grants the network gap exception, you’ll pay the lower in-network deductible, copay, or coinsurance for that particular out-of-network care. (source)
So, how do you take that extra step for your insurance to consider your surgeon in-network so that your surgeon and insurance can arrange a financial contract for payment?
It requires only filling out one form.
This form can be named any of the following:
clinical gap exception,
out-of-network exception,
network insufficiency exception,
gap waiver, or
network gap exception form.
You can obtain this form while you get your preauthorization form from your insurance. And to obtain this form, call your insurance first and request it. You might also be able to go online into their portal, but find out from your insurance to make sure.
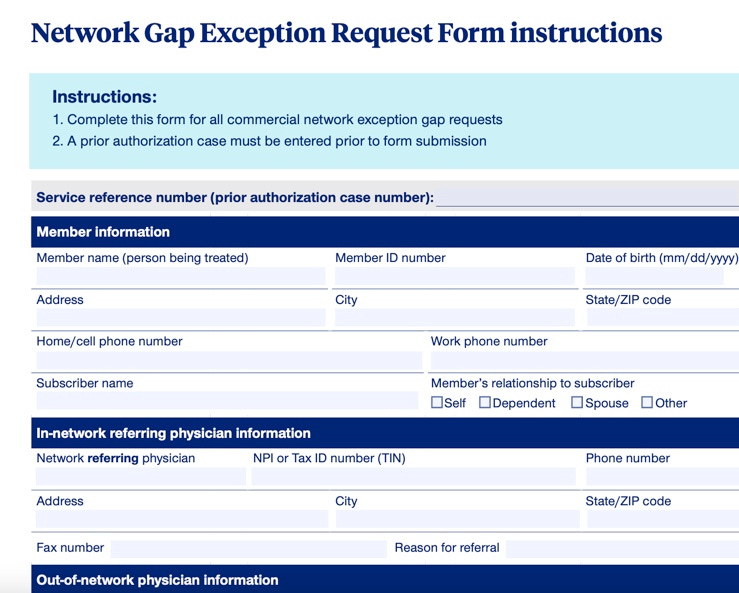
This (partial) form is from United Health Care. UHC has some rules that are different from most others, and if you read the top, this particular form states a prior auth must be submitted beforehand. However, you can sometimes submit your preauth and OON request at the same time.
Always check with your insurance if you can submit both preauth and OON submissions simultaneously or if you need to submit your OON after your preauth.
Let’s use this form below as an example:
Above is a real-life example of what an out-of-network exception form looks like. I pulled this form off the internet, a BCBS form for a particular plan in Montana.
As you can see, it is a basic form requiring demographic and surgeon/provider information.
Most of this form will be filled out by your surgeon. He will need to attach his surgical treatment plan and any other documentation to show why he should be considered for in-network reimbursement.
That is it! Your initial submission consists only of filling out this form and attaching supporting documentation. It is very straightforward. The. End.
Take care,
Michelle